Clinical Trail Audit Facility & Services
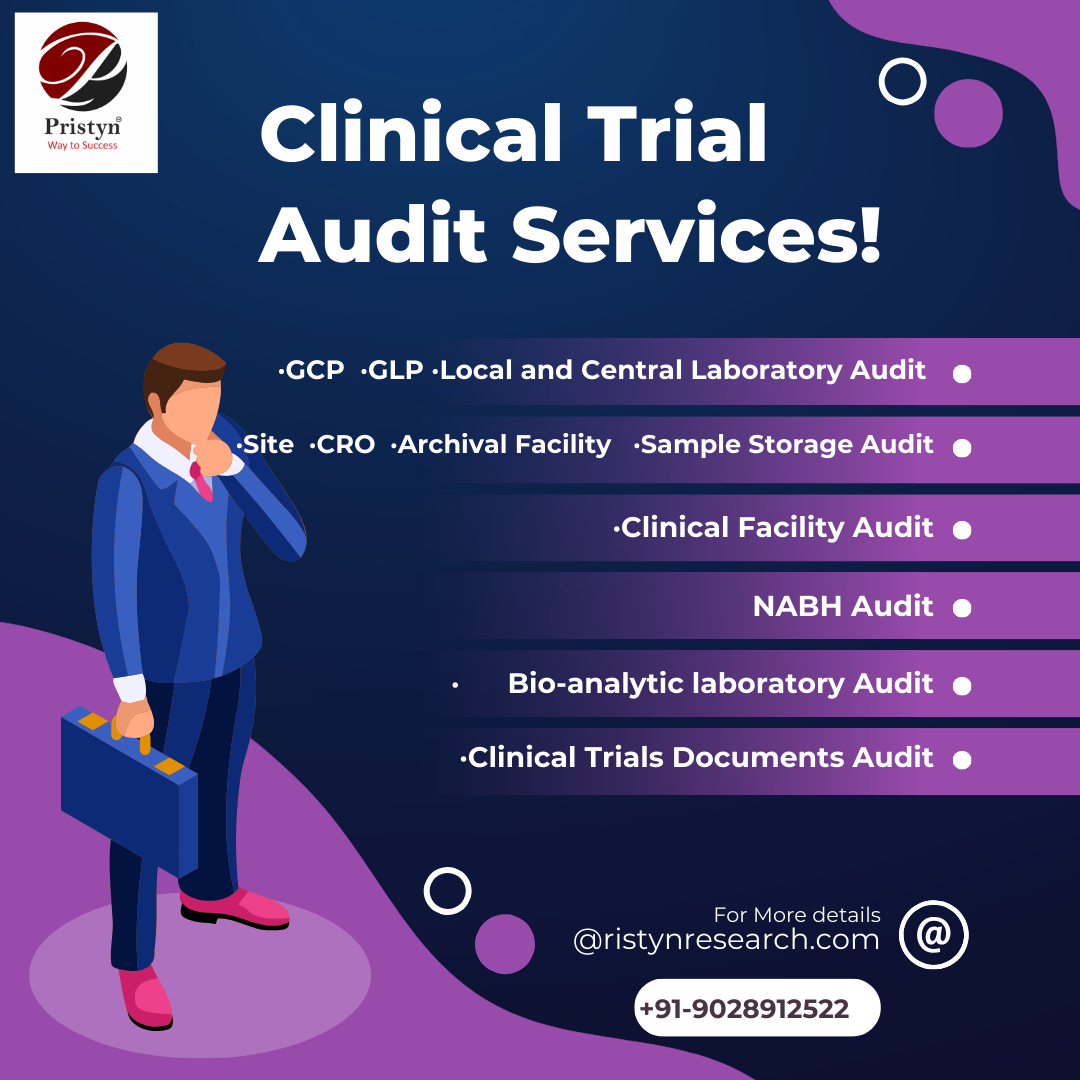
Clinical Trail Audit Facility & Services
The quality of data collected during a clinical trial greatly impacts its success. To ensure high-quality data, a comprehensive and well-organized system audit is crucial.
The quality of data collected during a
clinical trial greatly impacts its success. To ensure high-quality data, a
comprehensive and well-organized system audit is crucial. This audit helps
identify potential issues that may arise during the trial, and solutions can be
devised in advance to prevent any negative impact on the study. Different types
of audits can be conducted to ensure the accuracy and dependability of the
collected data, ultimately improving the success of the clinical trial.
In today's landscape of clinical trials and regulations, the process of designing and managing site audit programs has become increasingly complex. To ensure that audit objectives are met effectively, it is essential to have access to specialized expertise. This is where Pristyn Auditors come into play, leveraging their extensive knowledge and experience to provide comprehensive solutions for all your audit needs. Trust us to help you navigate the intricacies of this ever-evolving field.
- GCP Audit
- GLP Audit
- Local and Central Laboratory Audit
- Bio-analytic laboratory Audit
- Site Audit
- CRO Audit
- Archival Facility Audit
- Sample Storage Audit
- Clinical Facility Audit
GCP Audit
A Good Clinical Practice (GCP) audit is a systematic
process to evaluate and ensure that clinical trials are conducted in compliance
with ethical and regulatory standards. It involves reviewing trial
documentation, processes, and facilities to verify adherence to GCP guidelines.
Here's a step-by-step guide on how to conduct a GCP audit:
1.Preparation:
- Understanding GCP Guidelines: Familiarize yourself with the International Council for Harmonization (ICH) GCP guidelines and any applicable local regulations. These serve as the foundation for the audit.
- Define Audit Scope: Determine the scope of the audit, including specific trials, sites, or processes that will be assessed. Consider factors like trial phase, therapeutic area, and geographical location.
- Prepare Audit Plan: Develop a detailed audit plan that outlines the objectives, schedule, team members involved, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with the necessary expertise in GCP, clinical research, and the specific therapeutic area of the trials being audited.
- Independence: Ensure that the audit team members are independent from the trials being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, outline the objectives and scope of the audit, and establish expectations with the site personnel.
- Document Review: Review trial documentation including the Trial Master File (TMF), Informed Consent Forms (ICFs), Case Report Forms (CRFs), protocol, and regulatory submissions. Verify completeness, accuracy, and compliance with GCP.
- Site Visit: Conduct a physical visit to the trial site(s). Inspect facilities, ensure appropriate storage of investigational products, and observe the conduct of the trial.
- Interviews: Interview key site personnel including the Principal Investigator, sub-investigators, research coordinators, and other relevant staff. Discuss their roles, responsibilities, and understanding of GCP.
- Data Verification: Cross-check trial data from source documents to CRFs to ensure accuracy and consistency.
- Adherence to Protocol: Verify that the trial is being conducted according to the approved protocol.
- Safety Reporting: Review the handling and reporting of Serious Adverse Events (SAEs) and Adverse Events (AEs).
- Informed Consent Process: Assess the process of obtaining informed consent from participants, including documentation and communication of risks and benefits.
- Record Keeping: Evaluate the organization and completeness of trial records, including regulatory documents, source documents, and essential documents in the TMF.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the site personnel.
- Clarifications: Provide an opportunity for site personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in an audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited site. Ensure that they address the identified issues effectively.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, site responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited site are crucial throughout the audit process. It's important to approach the audit as a collaborative effort to improve the quality and integrity of clinical trials.
GLP Audit
A Good Laboratory Practice (GLP) audit is a thorough examination of a laboratory's processes, systems, and documentation to ensure compliance with established GLP standards. GLP ensures the reliability and validity of non-clinical safety studies.
Here's a step-by-step guide on how to conduct a GLP audit:
1.Preparation:
- Familiarize Yourself with GLP Standards: Understand the specific GLP standards and guidelines applicable in your jurisdiction. These may include OECD GLP, FDA GLP, EPA GLP, or other regional variations.
- Define Audit Scope: Determine the scope of the audit, including the specific studies, processes, or areas within the laboratory that will be assessed.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with expertise in GLP, laboratory operations, and the specific scientific disciplines relevant to the studies being audited.
- Independence: Ensure that the audit team members are independent from the studies being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Begin the audit with an entrance meeting to introduce the audit team, explain the audit objectives and scope, and establish expectations with the laboratory personnel.
- Document Review: Thoroughly review study documentation, including study protocols, Standard Operating Procedures (SOPs), raw data, reports, and quality control records.
- Laboratory Tour: Conduct a physical tour of the laboratory facilities. Inspect equipment, facilities, and storage areas for compliance with GLP standards.
- Interviews: Interview key laboratory personnel including study directors, analysts, Quality Assurance personnel, and management. Discuss their roles, responsibilities, and understanding of GLP.
- Data Verification: Cross-check study data, including raw data and calculations, to ensure accuracy, precision, and completeness.
- Adherence to Protocol: Verify that the studies are being conducted in accordance with the approved study protocols.
- Record Keeping: Evaluate the organization and completeness of laboratory records, including raw data, calculations, quality control records, and final reports.
- Equipment Calibration and Maintenance: Assess the calibration, maintenance, and validation status of laboratory equipment.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the laboratory personnel.
- Clarifications: Provide an opportunity for laboratory personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in a comprehensive audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited laboratory. Ensure that they effectively address the identified issues.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, laboratory responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited laboratory is crucial throughout the audit process. It's important to approach the audit as a collaborative effort to ensure compliance with GLP standards and to enhance the quality and reliability of non-clinical safety studies.
Local and Central Laboratory Audit
Auditing local and central laboratories is crucial to ensure that they are operating in compliance with regulatory requirements and industry standards. These audits help verify the accuracy, reliability, and integrity of laboratory results, which are essential for making informed decisions in clinical trials or other research endeavours.
Here is a step-by-step guide on how to conduct local and central laboratory audits:
1.Preparation:
- Understand Regulatory Requirements: Familiarize yourself with relevant regulatory guidelines and standards applicable to laboratory operations. This may include Good Clinical Laboratory Practice (GCLP), CLIA (Clinical Laboratory Improvement Amendments), and other regional or country-specific regulations.
- Define Audit Scope: Determine the scope of the audit, specifying whether it will focus on local or central laboratories. Additionally, identify specific areas or processes within the laboratory that will be assessed.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the Audit Team:
- Expertise: Assemble a team with expertise in clinical laboratory operations, regulatory compliance, and the specific scientific disciplines relevant to the studies being audited.
- Independence: Ensure that the audit team members are independent from the laboratories being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, explain the audit objectives and scope, and establish expectations with the laboratory personnel.
- Document Review: Thoroughly review laboratory documentation, including SOPs, equipment calibration records, quality control data, validation reports, and proficiency testing results.
- Laboratory Tour: Conduct a physical tour of the laboratory facilities. Inspect equipment, facilities, and storage areas for compliance with regulatory and industry standards.
- Interviews: Interview key laboratory personnel including laboratory managers, quality managers, analysts, and technicians. Discuss their roles, responsibilities, and understanding of regulatory compliance.
- Data Verification: Cross-check laboratory data, including raw data and calculations, to ensure accuracy, precision, and completeness.
- Adherence to SOPs: Verify that laboratory operations are conducted in accordance with approved SOPs and that deviations are appropriately documented and managed.
- Quality Control Measures: Evaluate the effectiveness of the laboratory's quality control measures in ensuring the accuracy and reliability of test results.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the laboratory personnel.
- Clarifications: Provide an opportunity for laboratory personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in a comprehensive audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited laboratory. Ensure that they effectively address the identified issues.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, laboratory responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited laboratory is crucial throughout the audit process. Approach the audit as a collaborative effort to ensure compliance with regulatory standards and enhance the quality and reliability of laboratory results.
Bio-analytical Laboratory Audit
A bio-analytical laboratory audit is a thorough assessment of a laboratory's processes, systems, and documentation related to the analysis of biological samples. These audits are essential to ensure compliance with regulatory requirements and industry standards, as well as the accuracy and reliability of bio-analytical data.
Here is a step-by-step guide on how to conduct a bio-analytical laboratory audit:
1.Preparation:
- Familiarize Yourself with Regulatory Requirements: Understand the specific regulatory guidelines and standards applicable to bio-analytical laboratories. These may include Good Laboratory Practice (GLP), Good Clinical Practice (GCP), and other relevant regional or country-specific regulations.
- Define Audit Scope: Determine the scope of the audit, including the specific studies, processes, or areas within the laboratory that will be assessed. Focus on bio-analytical methods, sample handling, and data reporting.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with expertise in bio-analytical laboratory operations, regulatory compliance, and the specific scientific disciplines relevant to the studies being audited.
- Independence: Ensure that the audit team members are independent from the studies being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Begin the audit with an entrance meeting to introduce the audit team, explain the audit objectives and scope, and establish expectations with the laboratory personnel.
- Document Review: Thoroughly review laboratory documentation, including bio-analytical method validation reports, sample handling procedures, raw data, data processing procedures, and final reports.
- Laboratory Tour: Conduct a physical tour of the laboratory facilities. Inspect equipment, facilities, and storage areas for compliance with regulatory and industry standards.
- Interviews: Interview key laboratory personnel including bio-analytical scientists, analysts, study directors, and quality managers. Discuss their roles, responsibilities, and understanding of regulatory compliance.
- Bio-analytical Method Verification: Verify that bio-analytical methods are validated and that validation parameters (e.g., specificity, accuracy, precision) meet regulatory requirements.
- Sample Handling and Storage: Evaluate the procedures for sample receipt, storage, tracking, and disposal. Ensure that they comply with GLP and GCP standards.
- Data Integrity and Processing: Review the procedures for data processing, including data entry, integration, and calculation of concentrations. Ensure that they are accurate and consistent.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the laboratory personnel.
- Clarifications: Provide an opportunity for laboratory personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in a comprehensive audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited laboratory. Ensure that they effectively address the identified issues.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, laboratory responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited laboratory is crucial throughout the audit process. Approach the audit as a collaborative effort to ensure compliance with regulatory standards and enhance the quality and reliability of bio-analytical data.
Site Audit
A clinical trial site audit is a comprehensive assessment of a clinical research site's processes, documentation, and compliance with regulatory requirements and GCP (Good Clinical Practice) guidelines. These audits are essential to ensure the integrity, quality, and safety of clinical trial data.
Here is a step-by-step guide on how to conduct a clinical trial site audit:
1.Preparation:
- Familiarize Yourself with GCP Guidelines: Understand the International Council for Harmonisation (ICH) GCP guidelines and any applicable local regulations. These serve as the foundation for the audit.
- Define Audit Scope: Determine the scope of the audit, including specific trials, processes, or areas within the site that will be assessed. Consider factors like trial phase, therapeutic area, and geographical location.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with the necessary expertise in clinical research, GCP, and the specific therapeutic area of the trials being audited.
- Independence: Ensure that the audit team members are independent from the trials being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, outline the objectives and scope of the audit, and establish expectations with the site personnel.
- Document Review: Review trial documentation including the Trial Master File (TMF), Informed Consent Forms (ICFs), Case Report Forms (CRFs), protocol, and regulatory submissions. Verify completeness, accuracy, and compliance with GCP.
- Site Visit: Conduct a physical visit to the trial site. Inspect facilities, ensure appropriate storage of investigational products, and observe the conduct of the trial.
- Interviews: Interview key site personnel including the Principal Investigator, sub-investigators, research coordinators, and other relevant staff. Discuss their roles, responsibilities, and understanding of GCP.
- Data Verification: Cross-check trial data from source documents to CRFs to ensure accuracy and consistency.
- Adherence to Protocol: Verify that the trial is being conducted according to the approved protocol.
- Safety Reporting: Review the handling and reporting of Serious Adverse Events (SAEs) and Adverse Events (AEs).
- Informed Consent Process: Assess the process of obtaining informed consent from participants, including documentation and communication of risks and benefits.
- Record Keeping: Evaluate the organization and completeness of trial records, including regulatory documents, source documents, and essential documents in the TMF.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the site personnel.
- Clarifications: Provide an opportunity for site personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in an audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited site. Ensure that they address the identified issues effectively.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the Audit:
- Final Report: Issue a final audit report summarizing the initial findings, site responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited site is crucial throughout the audit process. Approach the audit as a collaborative effort to ensure compliance with GCP guidelines and to enhance the quality and integrity of clinical trial data.
CRO Audit
A CRO audit is a comprehensive evaluation of a Contract Research Organization's processes, systems, and documentation to ensure compliance with regulatory requirements and industry standards. These audits are crucial for maintaining the quality, integrity, and reliability of clinical trial data.
Here is a step-by-step guide on how to conduct a CRO audit:
1.Preparation:
- Understand Regulatory Requirements: Familiarize yourself with relevant regulatory guidelines, including ICH-GCP, local regulations, and any specific requirements for the therapeutic area of the trials.
- Define Audit Scope: Determine the scope of the audit, including specific trials, processes, or areas within the CRO that will be assessed. Consider factors like trial phase, therapeutic area, and geographical location.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the Audit Team:
- Expertise: Assemble a team with expertise in clinical research, GCP, and the specific therapeutic area of the trials being audited. Additionally, individuals with experience in auditing or quality assurance are valuable.
- Independence: Ensure that the audit team members are independent from the trials being audited and have no conflicts of interest.
3.Conducting the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, outline the objectives and scope of the audit, and establish expectations with the CRO personnel.
- Document Review: Review trial documentation including the Trial Master File (TMF), Informed Consent Forms (ICFs), Case Report Forms (CRFs), protocol, and regulatory submissions. Verify completeness, accuracy, and compliance with GCP.
- Interviews: Interview key CRO personnel including project managers, clinical research associates (CRAs), data managers, and quality assurance professionals. Discuss their roles, responsibilities, and understanding of GCP.
- Data Verification: Cross-check trial data from source documents to CRFs to ensure accuracy and consistency.
- Adherence to Protocol: Verify that the trial is being conducted according to the approved protocol.
- Safety Reporting: Review the handling and reporting of Serious Adverse Events (SAEs) and Adverse Events (AEs).
- Quality Management System: Evaluate the CRO's quality management system, including SOPs, training records, and CAPA (Corrective and Preventive Action) processes.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the CRO personnel.
- Clarifications: Provide an opportunity for CRO personnel to ask questions or seek clarification on any findings.
5. Audit Report and Findings:
- Report Compilation: Document all findings, observations, and recommendations in an audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited CRO. Ensure that they address the identified issues effectively.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the Audit:
- Final Report: Issue a final audit report summarizing the initial findings, CRO responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited CRO is crucial throughout the audit process. Approach the audit as a collaborative effort to ensure compliance with GCP guidelines and to enhance the quality and integrity of clinical trial data.
Archival Facility Audit
An archival storage facility audit in clinical research is a thorough examination of a facility responsible for storing essential documents related to clinical trials. The purpose of this audit is to ensure that the facility maintains proper conditions for document preservation, security, and accessibility.
Here is a step-by-step guide on how to conduct an archival storage facility audit:
1.Preparation:
- Understand Regulatory Requirements: Familiarize yourself with the relevant regulatory guidelines and standards for document retention in clinical research. These may include ICH-GCP, FDA regulations, and local requirements.
- Define Audit Scope: Determine the scope of the audit, including specific documents, processes, or areas within the archival storage facility that will be assessed. Focus on aspects like storage conditions, access controls, and document retention policies.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with expertise in document management, regulatory compliance, and clinical research. Knowledge of archival practices is essential.
- Independence: Ensure that the audit team members are independent from the facility being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, outline the objectives and scope of the audit, and establish expectations with the facility personnel.
- Document Review: Thoroughly review the facility's documentation, including document retention policies, environmental monitoring records, security protocols, and access logs.
- Facility Tour: Conduct a physical tour of the archival storage facility. Inspect environmental controls (e.g., temperature, humidity), security measures (e.g., access controls, surveillance), and storage conditions.
- Interviews: Interview key personnel responsible for managing the archival storage facility. Discuss their roles, responsibilities, and understanding of document preservation requirements.
- Document Retrieval Process: Evaluate the process for retrieving stored documents. Ensure that it is well-documented, controlled, and allows for timely access when needed.
- Security Measures: Assess the security measures in place to protect documents from theft, loss, or unauthorized access. This includes physical security and electronic access controls.
- Environmental Monitoring: Verify that the facility monitors and maintains appropriate environmental conditions for document preservation (e.g., temperature, humidity).
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the facility personnel.
- Clarifications: Provide an opportunity for facility personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in an audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited facility. Ensure that they address the identified issues effectively.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, facility responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Remember, effective communication and collaboration with the audited facility is crucial throughout the audit process. Approach the audit as a collaborative effort to ensure compliance with regulatory standards and to enhance the security and accessibility of essential documents in clinical research.
Sample Storage Audit
A sample storage facility audit in clinical research is a thorough examination of a facility responsible for storing biological samples collected during clinical trials. The purpose of this audit is to ensure that the facility maintains proper conditions for sample preservation, security, and traceability.
Here is a step-by-step guide on how to conduct a sample storage facility audit:
1.Preparation:
- Understand Regulatory Requirements: Familiarize yourself with the relevant regulatory guidelines and standards for sample storage in clinical research. These may include ICH-GCP, FDA regulations, and local requirements.
- Define Audit Scope: Determine the scope of the audit, including specific samples, processes, or areas within the storage facility that will be assessed. Focus on aspects like storage conditions, access controls, and sample tracking.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with expertise in sample management, regulatory compliance, and clinical research. Knowledge of sample handling and storage practices is essential.
- Independence: Ensure that the audit team members are independent from the facility being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, outline the objectives and scope of the audit, and establish expectations with the facility personnel.
- Document Review: Thoroughly review the facility's documentation, including sample storage procedures, environmental monitoring records, security protocols, and sample inventory logs.
- Facility Tour: Conduct a physical tour of the sample storage facility. Inspect environmental controls (e.g., temperature, humidity), security measures (e.g., access controls, surveillance), and storage conditions.
- Interviews: Interview key personnel responsible for managing the sample storage facility. Discuss their roles, responsibilities, and understanding of sample preservation requirements.
- Sample Retrieval Process: Evaluate the process for retrieving stored samples. Ensure that it is well-documented, controlled, and allows for timely access when needed.
- Security Measures: Assess the security measures in place to protect samples from theft, loss, or unauthorized access. This includes physical security and electronic access controls.
- Environmental Monitoring: Verify that the facility monitors and maintains appropriate environmental conditions for sample preservation (e.g., temperature, humidity).
- Sample Inventory Management: Ensure that there is a robust system for tracking samples, including unique identifiers, labelling, and accurate inventory records.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the facility personnel.
- Clarifications: Provide an opportunity for facility personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in an audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited facility. Ensure that they address the identified issues effectively.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, facility responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Requirements for
Sample Storage in Clinical Research:
The requirements for sample storage in clinical research are critical to ensure the integrity, quality, and traceability of biological samples. Here are key requirements:
1.Proper Environmental Conditions:
Maintain appropriate temperature and humidity levels to ensure sample stability. This is particularly crucial for sensitive samples.
2.Secure Storage Facilities:
Implement robust physical security measures, such as access controls, surveillance, and intrusion detection systems, to protect samples from unauthorized access or theft.
3.Sample Tracking and Inventory:
Utilize a comprehensive system for sample tracking, including unique identifiers, labeling, and accurate inventory records. This ensures traceability and prevents sample mix-ups.
4.Documentation and Record-keeping:
Maintain thorough and accurate records of sample storage conditions, handling procedures, and any deviations or incidents. This documentation is crucial for audit trails.
5.Sample Retrieval Procedures:
Establish clear and documented procedures for retrieving samples when needed for analysis or further processing. These procedures should ensure sample integrity and traceability.
6.Monitoring and Alarming:
Implement a system for continuous environmental monitoring within the storage facility. This includes alarms for out-of-range conditions that could compromise sample integrity.
7.Emergency Response Plan:
Have a well-defined plan in place for responding to emergencies, such as power outages or equipment failures, to prevent any compromise of sample integrity.
8.Training and Competency:
Ensure that personnel involved in sample handling and storage receive appropriate training and are competent in following established procedures.
9.Quality Management System:
Have a robust quality management system in place, including Standard Operating Procedures (SOPs), to govern all aspects of sample storage.
10.Regulatory Compliance:
Adhere to all applicable regulatory requirements and guidelines for sample storage, including ICH-GCP, FDA regulations, and any local regulations.
11.Regular Maintenance and Calibration:
Conduct routine maintenance and calibration of equipment used for sample storage to ensure consistent and reliable environmental conditions.
12.Disaster Recovery Plan:
Develop a plan for recovering samples in the event of a disaster, such as a fire or natural disaster, to prevent loss of critical samples.
By adhering to these requirements, a sample storage facility can ensure that biological samples remain viable, reliable, and traceable throughout their storage period in clinical research.
Clinical Facility Audit
A clinical facility audit in clinical research is a comprehensive examination of a facility where clinical trials are conducted. The purpose of this audit is to assess whether the facility is compliant with regulatory requirements, follows Good Clinical Practice (GCP) guidelines, and maintains the highest standards of quality and safety in conducting clinical trials.
Here is a step-by-step guide on how to conduct a clinical facility audit:
1.Preparation:
- Understand Regulatory Requirements: Familiarize yourself with the relevant regulatory guidelines and standards for conducting clinical trials. These may include ICH-GCP, FDA regulations, and local requirements.
- Define Audit Scope: Determine the scope of the audit, including specific trials, processes, or areas within the facility that will be assessed. Focus on aspects like protocol compliance, patient safety, and documentation.
- Develop an Audit Plan: Create a detailed audit plan outlining the objectives, schedule, audit team members, and specific areas to be covered during the audit.
2.Selecting the
Audit Team:
- Expertise: Assemble a team with expertise in clinical research, GCP, and the specific therapeutic area of the trials being audited. Additionally, individuals with experience in auditing or quality assurance are valuable.
- Independence: Ensure that the audit team members are independent from the trials being audited and have no conflicts of interest.
3.Conducting
the Audit:
- Entrance Meeting: Start the audit with an entrance meeting to introduce the audit team, outline the objectives and scope of the audit, and establish expectations with the facility personnel.
- Document Review: Thoroughly review the facility's documentation, including trial protocols, Informed Consent Forms (ICFs), Case Report Forms (CRFs), regulatory submissions, and patient records.
- Site Visit: Conduct a physical visit to the clinical facility. Inspect facilities, ensure appropriate storage of investigational products, and observe the conduct of the trial.
- Interviews: Interview key facility personnel including the Principal Investigator, sub-investigators, research coordinators, and other relevant staff. Discuss their roles, responsibilities, and understanding of GCP.
- Patient Safety: Assess the measures in place to ensure patient safety, including adverse event reporting, monitoring for safety concerns, and compliance with the protocol.
- Data Integrity: Verify the accuracy and completeness of trial data, including source data verification.
- Regulatory Compliance: Evaluate the facility's compliance with regulatory requirements, including the timely submission of regulatory documents.
- Informed Consent Process: Assess the process of obtaining informed consent from participants, including documentation and communication of risks and benefits.
4.Exit Meeting:
- Objectives: Conduct an exit meeting to summarize the findings and observations with the facility personnel.
- Clarifications: Provide an opportunity for facility personnel to ask questions or seek clarification on any findings.
5.Audit Report
and Findings:
- Report Compilation: Document all findings, observations, and recommendations in an audit report. Clearly differentiate between major and minor findings.
- Recommendations: Include recommendations for corrective and preventive actions to address the identified issues.
6.Follow-Up:
- Corrective Actions: Monitor the implementation of corrective actions by the audited facility. Ensure that they address the identified issues effectively.
- Verification: Conduct a follow-up audit if necessary to verify that corrective actions have been implemented and are effective.
7.Closing the
Audit:
- Final Report: Issue a final audit report summarizing the initial findings, facility responses, and any follow-up actions taken.
- Archive Documentation: Ensure that all audit documentation, including the audit plan, report, and any correspondence, is appropriately filed and archived.
8.Maintaining
Independence and Impartiality:
Throughout the audit process, maintain independence and impartiality. Avoid conflicts of interest and ensure that the audit is conducted objectively.
9.Continual
Improvement:
Review the audit process and findings to identify areas for improvement in future audits. Incorporate lessons learned to enhance the effectiveness of future audits.
Requirements for
Clinical Facility Audit in Clinical Research:
The requirements for a clinical facility audit are critical to ensure the integrity, quality, and safety of clinical trials. Here are key requirements:
1.GCP Compliance:
The facility must adhere to Good Clinical Practice (GCP) guidelines, which are international ethical and scientific quality standards for the design, conduct, recording, and reporting of clinical trials.
2.Qualified Investigator:
The facility must have a qualified Principal Investigator responsible for the conduct of the clinical trials.
3.Ethics Committee Approval:
All trials conducted at the facility must have obtained prior approval from an independent ethics committee.
4.Informed Consent Process:
The facility must have a documented process for obtaining informed consent from participants, ensuring they fully understand the risks and benefits of participation.
5.Patient Safety Measures:
Adequate measures must be in place to monitor and ensure the safety of participants throughout the trial, including prompt reporting of adverse events.
6.Protocol Adherence:
The facility must ensure that the trial is conducted according to the approved protocol, with any deviations appropriately documented and justified.
7.Data Integrity and Documentation:
Accurate and complete data must be maintained, including source data and CRFs, to ensure the reliability and validity of trial results.
8.Regulatory Compliance:
The facility must comply with all applicable regulatory requirements, including timely submission of regulatory documents.
9.Storage of Investigational Products:
Investigational products must be stored in accordance with manufacturer specifications and regulatory requirements.
10.Record Keeping:
Thorough and accurate records must be maintained, including regulatory documents, source documents, and essential documents in the Trial Master File (TMF).
11.Training and Competency:
Personnel involved in the conduct of clinical trials must be adequately trained and competent in their respective roles.
12.Quality Management System:
The facility must have a robust quality management system in place, including Standard Operating Procedures (SOPs), to govern all aspects of clinical trial conduct.
By adhering to these requirements, a clinical facility can ensure that clinical trials are conducted with the highest standards of quality, safety, and ethical conduct, thereby safeguarding the rights and well-being of trial participants and producing reliable data for regulatory submission.
